Inhuman trials
 yet another instance of outsourcing of high-risk clinical drug trials has been brought to light by a child specialist of a reputed hospital in New Delhi. The doctor recently told Down To Earth (dte) that in August last year, Mumbai-based contract research organisation Siro Clinpharm Private Limited asked him to arrange for newborn babies to test an immune globulin for hepatitis manufactured by Canadian biotechnology company Cangene Corporation.
yet another instance of outsourcing of high-risk clinical drug trials has been brought to light by a child specialist of a reputed hospital in New Delhi. The doctor recently told Down To Earth (dte) that in August last year, Mumbai-based contract research organisation Siro Clinpharm Private Limited asked him to arrange for newborn babies to test an immune globulin for hepatitis manufactured by Canadian biotechnology company Cangene Corporation.
"For doing this, I was to be compensated at the rate of Rs 38,000 per baby recruited. While I turned down the offer, the company can easily attract others with this kind of money,' the doctor told dte. Last heard, the trials were indeed in progress in India, with one of the sites being a Hyderabad government hospital.
Of late, numerous foreign entities have gained easy access to unsuspecting patients in India and dished out the guinea pig treatment to them. A case in point is the controversial cancer drug trial funded by the us-based Johns Hopkins University and carried out at Kerala's Regional Cancer Centre. Gopalan, the last survivor of that experiment, died on June 15. What is alarming is that despite such bitter experiences, the country's already lax rules in this regard might be diluted further.
Dubious research? Cangene's protocol booklet mentions that it would carry out trials of an immune globulin for hepatitis in 15 sites across Canada and India. The drug was to be tested on newborn babies of hepatitis-positive mothers. All infants were given standard hepatitis b vaccine along with the new experimental immunoglobin. Hepatitis b is passed on from mother to child during birth, and the product was to be administered to ascertain whether it could enhance the activity of the vaccine.
The Delhi doctor alleges that the experiment's protocol is flawed. Even though the booklet notes that the hepatitis b vaccine provides 70-95 per cent protection, the study is being conducted to verify if the protection provided by the immunoglobin is more than 92 per cent. In effect, the company wants to declare the immunoglobin useful, despite its potency being less than that of the hepatitis b vaccine alone. Furthermore, the product is being tested without any information on how the disease behaves in Indians.
But Siro's senior manager, strategic planning and clinical operations, Ajit Nair, specifies: "The drug controller general and all the institutional ethics committees have given a clearance to the Cangene protocol.' Meanwhile, dte's repeated attempts to get Cangene's response proved futile.
The onus to ensure that the tests are conducted in a fair manner is on the ethics committees of research institutes. But a recent survey published in the Journal of Medical Ethics shows that a quarter of the clinical trials conducted in developing countries do not even undergo ethical review. Often, drug companies bribe ethics panels, say experts.
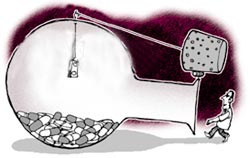
Lucrative proposition Drug companies outsource clinical trials to developing countries in order to cut costs. This is because it is unlikely that poor patients, who are generally chosen as the subjects in such experiments, would be able to litigate if they suffer adverse reactions.
Cangene's consent form for its study states that if the baby or the mother sustains a physical injury as a result of the procedure, the study doctor will provide the necessary treatment. It further specifies that the drug company shall not be liable to pay any form of additional financial compensation. Experts say that many drug companies do not divulge the risks involved in such trials.
"This is totally against the Helsinki Declaration (on ethical principles for medical research), which states that trials should be carried out without harming the human subject,' points out Chandra M Gulhati, editor of journal Monthly Index of Medical Specialities . The declaration also states that vulnerable sections or those which may not benefit from the product should not be used for drug trials. This guideline seems to have been ignored in the case in question. There is also the problem of lack of transparency in most clinical trials, where information about the tests is not made available in the public domain.
The legal position In India, clinical tests are controlled by schedule y of the Drugs and Cosmetics Act of 1940. In its present form, the regulation stipulates that a trial phase can begin in the country only after it has been completed successfully elsewhere. But in August 2003, a plan was chalked out to allow concurrent clinical trials in India and the country of the drug's origin. However, this proposal is yet to be tabled in parliament.
Experts are worried that the proposed changes to the law may permit drug companies to study just one fully insured case from developed countries like usa and 99 from India with minimal insurance. But the Drug Controller General of India, Ashwini Kumar, feels that India is losing out on drug development research due to misinformation.
