Borne again
 ALMOST 100 years after the discovery of the mosquito-bornemalarial parasite by Sir Ronald Ross in 1897scientists andpublic health experts are still grappling with ways to tackle thekiller disease. According to World Health Organization (WHO)estimatesmalaria afflicts about 500 million people annuallythe world over; 90 per cent of the cases occur in Africa aloneand the rest mainly in India (40 per cent of all malaria casesoutside Africa)BrazilSri LankaAfghanistanThailandVietnam and Colombia. The disease claims about 2.7 millionlives annuallyincluding an estimated one million Africanchildren under five.
ALMOST 100 years after the discovery of the mosquito-bornemalarial parasite by Sir Ronald Ross in 1897scientists andpublic health experts are still grappling with ways to tackle thekiller disease. According to World Health Organization (WHO)estimatesmalaria afflicts about 500 million people annuallythe world over; 90 per cent of the cases occur in Africa aloneand the rest mainly in India (40 per cent of all malaria casesoutside Africa)BrazilSri LankaAfghanistanThailandVietnam and Colombia. The disease claims about 2.7 millionlives annuallyincluding an estimated one million Africanchildren under five.
Malaria eradication was believed to be at hand in the '50sand '60sbut widespread resistance to drugs and insecticidesled to a resurgence. Dreams of eradication gave way to pragmatic "strategies for control"then were scaled down to just.'managing epidemics". Obviouslythe single-celled parasiteand its fragile looking vector (the mosquito) have stayed onestep ahead of every human effort to combat them.
In Indiafigures released by the National MalariaEradication Programme (NMEP) show that while the incidenceof malaria has stabilised at about two-2.5 million cases peryeardeaths due to the disease have been increasing steadilyclaiming over 10lives annually since 1994.
Howeverhealth professionals believe that the true numbers of both the stricken and the dead may be anywherebetween five- 10 times the official figures. The last two yearshave seen major outbreaks in GujaratRajasthanthe north-east and West Bengal. "The important thing is not how manypeople diedbut why should anyone have to die of a preventable and trettable disease like malariasays Mira Shiva, health activist and policy expert, Voluntary Health Association of India (VHAI), New Delhi.
According to experts, the situation is likely to deteriorate further with the virtual collapse of public health institutions, inaccessibility to primary health care, increasing poverty, shrinking health budgets, improper surveillance, irrational use of drugs and insecticides, lack of information, education and intersectoral coordination, high mobility of population from or to malarious areas, mismanagement and corruption in control measures, and, most importantly, continued tendency to ignore the public health aspects of developmental projects which often create malariogenic conditions.
India's entire population (with the exception of about 15 million people living at high altitudes of above 5,000 feet) is susceptible to malaria. But tribals, children and pregnant / lactating women stand a higher risk. A recent study in Orissa's Keonjhar district showed that nearly six per cent of all pregnant women and eight per cent of pre-school children suffer from malaria at any point of time, and that malaria claimed responsibility for over 50 per cent of all deaths in the district. Blood bugs
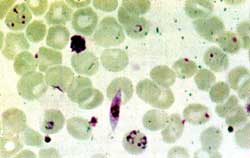
Malaria is a disease of red blood cells (RBC). It is caused by a protozoan parasite, the Plasmodium (P vivax, Pfalciparuni, P malariae and P ovale- the fist two are mainly responsible for malaria in India) and is transmitted by female Anopheles mosquitoes. About 51 species of the genus Anopheles are found in India, nine of them malaria carriers.
Species of Plasmodium Lown to infect birds, monkeys and mice are used as model systems by researchers for studying the disease.But host specificity is very high amongPlasmodium species. You cannot grow vivax in monkey ormicesays V S Chauhan, a malaria expert at the International Centre for Genetic Engineering and Biotechnology, New Delhi.
Scientists at New Delhi's Malaria Research Centre (MRC) have recently discovered that not all sub-species within each vector species are carriers.For exampleAn culicifaciestheMain vector for rural malariahas four sibling species - ABc and D. Of theseonly A is a strong vectorsays V P Sharma, director, MRC.
The disease is transmitted when an infected mosquito bites a healthy human host, and occasionally through blood transfusions (see diagrammatic representation: pages 30-31). Sporozoites (a stage in the parasite's life-cycle) invade the liver cells, multiplying and maturing into merozoites in six to eight days. During this process, the disease has no clinical manifestations.
In the next stage, thousands of merozoites burst forth from each liver cell and join the bloodstream, attacking the RBc and multiplying asexually. Symptoms appear during this stage, and the microscopic study of blood smears reveals the parasite. Some merozoites mature into gametocytes in the human RBc and when picked up by the mosquito, reproduce sexually in its stomach. The sporozoites produced in this manner reach the salivary glands of the insect, from where they infect the next human host. The entire process of development of the parasite in the mosquito takes about 10- 12 days.
Clinically, there are two types of malaria. The most common, vivax malaria, is benign but recurs unless treated effectively. The other type is falciparurn malaria, commonly called malignant or cerebral malaria, which is dangerous, even fatal. The RBc become sticky, forming lumps which may block the capillaries, arresting blood supply to different organs. If this happens in the brain, coma and eventual death follows.
Malaria is usually accompanied by anaernia and enlargement of the spleen. Hyperpyrexia (persistent high temperatures), another disorder, can cause febrile fits and brain dam- age. Occasionally, destruction Of RBC can lead to hypoxia - (reduced oxygen supply to the tissues). Malaria can also seriously jeopardise the outcome of pregnancy: the chances of abortion) low birth weight, still births and complications during delivery are enhanced.
The resistance syndrome
According to V P Sharma, several states have reported instances of falciparum with advanced resistance to chloroquine. Resistance to sulphalene / sulphadoxine and pyrimethamine groups of drugs, amodiaquine, mefloquine, a banned drug sold unofficially, and quinine, the ultimate choice in complicated cases, is also on the rise.
Resistance to insecticides like DDT is common; malathion and dieldrin have joined the list as well. Recent reports in the Indian Journal of Malariology reveal that resistance to even multiple insecticide combinations is developing. Synthetic pyrethroids (insecticides which do not have long-term residual effects) such as lambdacyhalothrin are known to be more effective and environmentally safer than insecticides in use, but their cost is prohibitive. Chemical larvicides such as paris green, temephos or fenthion and biological larvicides such as the bacteria, Bacillus thuringenesis and B sphericus can also be sprayed over water bodies. Formulations of biolarvicides, developed and field-tested by the MRc and NMEP, were recently cleared for use in mosquito control. The rot within
Experts attribute malaria's resurgence mainly to the failure of peripheral public health institutions. About 40 per cent of posts in India's health care centres lie vacant, according to V P Sharma. NMFP officials say that most primary health care centres (PHCS) do not have microscopes in working order. Even in fully functional PHcs, blood slides accumulate for four-six weeks, delaying diagnosis and radical treatment. In most villages, the drug distribution centres and fever treatment depots for malaria care are either non-existent or defunct.
Insecticide spraying operations are either not conducted, or are incomplete or ineffective in terms of the choice of the insecticide, area covered, number of required rounds and adulteration. The collapse of the health surveillance system has resulted in adhocism. Funding for malaria research is in a worse bind. Under the NMEP'S modified plan of operation (1977), malaria control costs came to be shared equally by the Centre and the states.
The subsidy cuts under the structural adjustment programme brought budgetary allocation down to Rs 72.45 crore in 1991-92, and to Rs 50 crore in 1992-93. Subsequently, the allocation was increased to Rs I 10 crore, but included programmes for kala azar, filaria, Japanese encephalitis and guinea worm as well. The Union government is currently negotiating a us $140 million World Bank loan to fight malaria in the metros and tribal areas.
D Banerjee, public health expert and professor emeritus at the Centre for Social Medicine and Community Health, Jawaharlal Nehru University, New Delhi, says,Unpardonableacts of omission and commissionby the political leadership ...have led to a sharp decline inthe quality of public healthservices... When there was anoutbreak of malaria in Rajasthanin 1994the malaria controlmachinery of the state wasalmost non-existent in theaffected villages... theafflictedpeople had to Cry Out to NGOSfor help." VHAi activists pointout that health officials tendto suppress malaria incidencefigures (during the 1994Rajasthan epidemicthe officialfigureof annual parasite index was0.59independent surveys'showed this to be above 5.0).
What's being done
A country-wide review of malariacontrol strategies wasundertaken in 1995followingwhich a Malaria ActionProgramme (MAP) was launched.Under MAP'high risk' ruraland urban areas were identifiedfor accelerated control measuresdrug policies andtreatment schedules. Vectorcontrolmeasures were revisedwithemphasis on appointment of voluntary link workers at thevillage levelupgradation offacilitiesand intersectoral coordination.But experts point out thatmany of the changes - selectiveinsecticide sprayingfor one- suggested under MAP aretechnical and shortsighted.
In keeping with India'scommitment to the October 1992WHO global malaria controlstrategythe government draftedanational malaria controlstrategy in 1995. The newstrategyemphasises decentralisationepidemiological approaches in malaria controlcommunity participationmanagementinformation systems and health educationamong other things.
Till datethe responsibility for malaria control in the entirecountry had mostly rested with the NMEP. Under the proposednew strategythe financialtechnical and administrativeresponsibilities will be shared by major establishments in- theprivate and public sectorssuch as megaprojectstea / coffeeplantationsirrigation projects or railways / airports / seaports. The NMEP and MRc directors and V S Orlov of the WHO hadjointly recommended in 1994 that health impact assessmentbe made an integral part of the environmental impact assessment of all developmental projects.
Malaria research has several aspects: developing newdrugsvaccinessimple diagnostic methodsinsecticides andlarvicidesmethods of sterilising mosquitoesepidemiologicaland entomological studieshost-parasite interactionsimmunology of the disease andfinallyecology.
Experts strongly argue for bio -environmental control ofmosquito breeding by spraying larvicidal microbesorthrough fish species such as gambusia or the gupp MRC Scientists have identified at least four other species of fishtheDanio rerioAplocheilus panchaxOryzias melastigma andAapia mossambica which are known to feed on mosquito tar -vae. Combining mosquito control with rearing fish for consumption and profit has yielded encouraging results.Moreoverthe estimated cost of biocontrol could be as low asRs 4.97 per capita per yearas compared to Rs 6 using chemical insecticides.
Impregnated bednets are being increasingly recommendedfor malaria controlfollowing encouraging results in Orissaand the north-east. These bednets are impregnated twice ayear with synthetic pyrethroidsoffering effective protectionfor six-eight months from mosquitoesbedbugs and headlice.
Among the new drugs waiting to be introduced in themarket is a Chinese herb derivativeArtemisia annuapopularly known as Qinghaosu in China. Artemisinthe raw material.was identified as a potent antimalarial and analysed in Chinain 1972. Introduced by WHO in VietnamThailand and Cambodiait successfully curedmulti- drug- resistant malariacases. Another Chinese herbaldrugPyronaridinehas beenfound to be 100 per centeffective in the early stages ofmalariaaArding to a report in TheLancet (January 1996).
In Indiaclinical trials ofArteethera derivative developedby the Central Drug ResearchInstitute (CDRI)Lucknowarecurrently underway. The CentralInstitute of Medicinal andAromatic Plants (CIMAP)again inLucknowhas successfullyadapted the plant for cultivationin Indiaand also developedan improved method for extractingarternisinic acid and converting it into artemisinpavingthe way for its indigenouscommercial production. A WHOcommittee has recommendedthat in order to avoiddevelopment of resistance toartemisinits use should be restricted toonly those regions where multiple drug resistance is rampant.
Indigenous production and sale ofmefloquin was clearedby the government in March thisyear. The technology for theproduction of the drug is alreadyavailable with the IndianInstitute of Chemical TechnologyHyderabad.
The MRC is currently conductingclinical trials for a drugdeveloped by the CDR1. The drugcodenamed Compound80has been found to beeffective in curing monkey malaria; the results of human trialsare awaited. MRC scientists arealso assessing the antimalarialproperties of a wild herb fromBastarMadhya Pradeshlocallycalled bhuineem. The Centrehas applied remote sensing andgeographical information systems to identify malariatransmission conditions inGujarat's Kheda district.
Indian Council of MedicalResearch scientists at Port BlairAndaman & Nicobar Islandshaverecently found a plant thatis used by the local Onge tribeand could provide yet anotherweapon to fight malaria. -But thecontroversy on intellectualproperty rights over the plantproduct is likely to delay itsinduction into the antimalariaprogramme.
Scientists at the IndianInstitute of ScienceBangaloreareworking on a drug which attacksthe heme biosynthetic pathway of the P berghei which causesmouse malaria. According todirector G Padmanabhanthefinding may help in fightinghuman malaria too. Ais team hasalso developed a diagnostickit in collaboration with AstraResearch CentreBanglorebased on non-radioactivedetection Of DNA of the parasiteinblood samples without amicroscope.
Bangalore University's Centre for Applied Geneticsresearchers have taken adifferent route to beat malaria -bygenetically modifying mosquitoesso that they cannot breed.According to director N J Shettythey have already succeededin inducing genetic sterility inthe male Anopheles (Anstephansi and An fluviatilis).The researchers have alsoidentified a strain of femaleAnopheles that is resistant to themalarial parasiteand the genethat imparts this resistance.
The idea of controlling malariathrough genetically engineered mosquitoes dates back toChris Curtis' (of the LondonSchool of Hygiene and TropicalMedicine) efforts in the '60s.Laboratories in many countriesare still pursuing the idea.Howeverscientists such asAndrew Speilman of HarvardUniversityUSAfeel that suchhi-tech approaches divertmoney and attention from the lessglamorous conventionalmethods. Indian scientists alsopoint out that research intoepidemiologyvector behaviourecology and public health arenot receiving adequate attention.
There are three major stages inthe life-cycle of the parasite which are targets for vaccine development:
• A vaccine based on sporozoites is designed to preventinfection.
• Vaccines based on the asexual blood stages of the parasite(merozoites) will not prevent infectionbut can reduce oreliminate parasites in the blood.
• Vaccines directed at the sexual stages of the parasite (gametocytes) aim to interfere with the ability of the parasite toinfect mosquitoes and thereby prevent transmission of thedisease.
Ideallya vaccine aprist malaria should contain all threefeaturesbut since the cell surface characteristics of each stageof the parasite are differentthat would be possible only froma 'cocktail' of antigens (cell surface proteins) of all stages. About 45 different proteins of the parasite have been identified so farof which about 15 are considered potential targetsfor vaccine development. A vaccine developed by a group ofAustralian researchers is undergoing trials since 1994 in USAand Africa.
According to V S Chauhanconventional vaccinesdesigned to generate antibodies against the parasite are notlikely to provide full protection. They also need to activate the'killer cells' (T-cells) of the human immune system.Fortunatelythe parasite does carry some markers on its cellsurface which can also activate these T-cells. Identifying andincorporating them into the 'final cocktail' will get the bestresults. Chauhan's team has identified some such markers. Asimilar strategy is being followed by researchers led by AdrianHill at the Institute of Molecular MedicineOxfordUK.
There are no magic bullets to beat malaria as yet. Settingaside eradicationbetter public health management practicesstrong primary health care infrastructure and emphasis onpreventive measures and community participation have thepotential to reduce malaria incidence and make the WHO'sdream of a one-fifth reduction in malaria incidence by 2000 AD- in at least 75 per cent of the affected countries - a reality.
